Genetically engineered immune cells successfully keep two people cancer-free for over a decade
February 10, 2022
Two blood cancer patients received an experimental immunotherapy in 2010, and their cancers went into remission. According to a report in Nature published Feb 2, the cancer-fighting immune cells used in the therapy were still around, over a decade later. This experimental treatment, known as CAR-T cell therapy uses genetically engineered versions of patients’ own immune cells to kill cancerous cells. Based on the results of this trial, “we can now conclude that CAR-T cells can actually cure patients with leukemia,” said cancer immunologist and study co-author Carl June of the University of Pennsylvania at a Feb 1 news briefing.
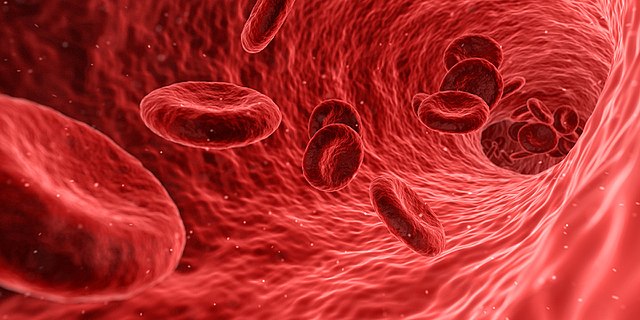
Researchers have tried for decades to engineer the immune system to fight cancer more effectively. “Immunotherapy goes back a long time, but successful immunotherapy is just in its infancy,” says Paul Martin, a pediatric oncologist at Duke University. CAR-T cell therapy works by taking advantage of how cells communicate with each other. The surface of every cell is covered in proteins that send messages between cells.
The engineered T cells have a synthetic receptor that only binds to a specific protein that appears on the surface of certain cancerous blood cells. The U.S. Food and Drug Administration approved two versions of CAR-T cell therapy in late 2017. In a clinical trial for Yescarta, a CAR-T treatment for adults with certain types of lymphoma, 51% of patients showed no sign of cancer after treatment. This result is promising because the patients in this trial were either dealing with a recurrence of cancer or did not respond favorably to at least two other treatments.
The biggest disappointment is that immunotherapy doesn’t work for anyone, said David Porter of the University of Pennsylvania. Some people don’t respond to the treatment and others can develop dangerous side effects. For example, the T-cells that are engineered to kill cancer cells could send the immune system into overdrive by sending a surge of proteins called cytokines into the bloodstream, triggering inflammation. This response is called Cytokine release syndrome and has been implicated in clinical trials of CAR-T cell therapies.
Many oncologists are still convinced that someday CAR-T cells could be used to treat a broader range of cancers. According to Science News, researchers across the world are already working on methods to improve CAR-T cell treatments, such as installing an off-switch for the genetically engineered T-cells in the form of a synthetic molecule or developing a universal CAR-T cell treatment that hospitals can carry in the same manner as pain medications.